Migraines are a debilitating condition affecting approximately 18% of the adult population in the United States. While migraines are often associated with triggers like stress, hormonal changes, or certain foods, recent studies suggest a potential correlation between migraines and insulin resistance. This emerging area of research offers valuable insights into why some people experience migraines and how addressing underlying metabolic issues could help reduce their frequency.
@thenewlifechannel♬ original sound – The New Life Channel
What Is Insulin Resistance?
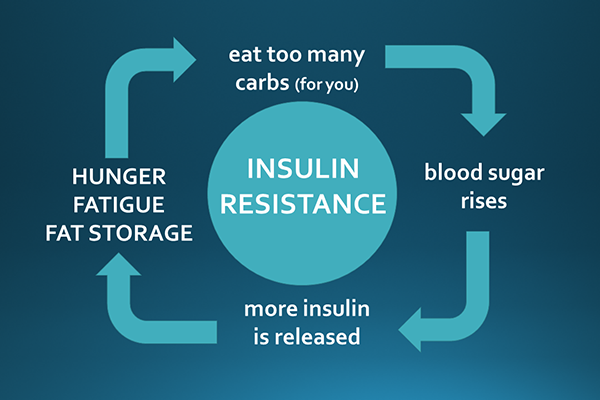
To understand the link between migraines and insulin resistance, it’s essential to first grasp what insulin resistance is.
Insulin is a hormone that helps regulate blood sugar (glucose) by allowing it to enter your cells for energy. When your body’s cells stop responding effectively to insulin, blood sugar levels remain elevated, and the pancreas compensates by producing even more insulin. Over time, this condition, known as insulin resistance, can lead to metabolic complications, including type 2 diabetes and increased inflammation—both of which are also linked to migraines.
Migraines: More Than Just a Headache

Migraines are not your average headaches. They are a neurological condition characterized by intense, throbbing pain that can last for hours or even days. Other common symptoms include:
- Nausea
- Sensitivity to light and sound
- Visual disturbances (aura)
- Difficulty concentrating
While the exact cause of migraines remains unclear, research has increasingly pointed to disruptions in brain metabolism and inflammation as contributing factors.
The Link Between Insulin Resistance and Migraines

A growing body of evidence suggests that insulin resistance may play a role in the development and frequency of migraines.
Higher Insulin Levels in Migraine Sufferers
A study comparing individuals with and without migraines found that insulin levels were significantly higher in those who experienced migraines. This indicates a potential metabolic component to the condition, where high insulin levels may contribute to the onset of migraine symptoms.
Glucose and Brain Function
The brain is one of the most energy-demanding organs in the body, relying on a steady supply of glucose for optimal function. In individuals with insulin resistance, glucose cannot efficiently enter the cells, including brain cells. This could leave the brain undernourished, potentially triggering migraines.
Reduced Migraine Frequency with Improved Insulin Sensitivity
In a study involving 32 participants who regularly experienced migraines, those treated with insulin-sensitizing medication saw a significant reduction in migraine frequency. This finding highlights the potential for addressing insulin resistance to mitigate migraine symptoms.
Why Insulin Resistance Could Trigger Migraines

Several mechanisms may explain how insulin resistance contributes to migraines:
- Inflammation
Insulin resistance is closely linked to chronic low-grade inflammation, which can sensitize nerve pathways and increase the likelihood of migraines. - Vascular Dysregulation
Insulin resistance may impair the function of blood vessels, leading to poor circulation in the brain. Reduced blood flow could exacerbate migraine symptoms. - Energy Deficiency in the Brain
Without sufficient glucose reaching the brain, due to insulin resistance, the brain may experience an energy deficit, triggering migraines. - Hormonal Disruptions
Insulin resistance affects other hormones, such as cortisol and estrogen, which are known migraine triggers.
Addressing Insulin Resistance to Reduce Migraines

If insulin resistance contributes to your migraines, improving insulin sensitivity could help reduce their frequency and severity. Here are some strategies to consider:
1. Adopt a Balanced Diet
- Limit processed foods and added sugars that spike insulin levels.
- Focus on whole, nutrient-dense foods like vegetables, lean proteins, and healthy fats.
- Incorporate foods high in fiber, which help stabilize blood sugar levels.
2. Practice Intermittent Fasting
Intermittent fasting can lower insulin levels and improve insulin sensitivity over time. By giving your body regular fasting periods, you allow it to reset and burn stored fat for energy, reducing inflammation and stabilizing blood sugar.
3. Stay Physically Active
Exercise enhances insulin sensitivity by helping your muscles absorb glucose more effectively. Activities like walking, cycling, and strength training can make a significant difference.
4. Get Quality Sleep
Poor sleep disrupts insulin regulation and increases stress hormones, which can exacerbate both insulin resistance and migraines. Aim for 7–9 hours of restful sleep per night.
5. Manage Stress
Chronic stress raises cortisol levels, which can worsen insulin resistance and trigger migraines. Incorporate stress-reducing practices like meditation, yoga, or deep breathing exercises into your daily routine.
What This Means for Migraine Sufferers

Understanding the connection between insulin resistance and migraines opens the door to new strategies for managing this debilitating condition. While traditional treatments often focus on pain relief, addressing the underlying metabolic dysfunction may provide longer-term benefits.
Next Steps

Migraines are complex, multifaceted conditions, but the potential link to insulin resistance offers hope for those seeking effective solutions. By improving your insulin sensitivity through lifestyle changes like diet, exercise, and intermittent fasting, you can take proactive steps to not only reduce the frequency of migraines but also enhance your overall health.
If you’re interested in learning more about how intermittent fasting can improve insulin sensitivity and help manage conditions like migraines, check out my blog: How Intermittent Fasting Helps You Lose Weight: A Complete Guide.
Don’t let migraines control your life. Start addressing the root causes today and take a step toward a healthier, pain-free future.
Your Thoughts Matter